|
Case Report
Postpartum acute pancreatitis in the setting of severe preeclampsia: Diagnostic challenges and surgical findings
1 Department Obstetrics and Gynecology, Tufts Medical Center, Boston, MA, USA
2 Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, Tufts Medical Center, Boston, MA, USA
Address correspondence to:
Marie Elise Abi Antoun
800 Washington Street, Boston, MA 02111,
USA
Message to Corresponding Author
Article ID: 100080Z09MA2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Abi Antoun ME, Kassem Z, Cammock EC, Lee CM, Craigo S. Postpartum acute pancreatitis in the setting of severe preeclampsia: Diagnostic challenges and surgical findings. J Case Rep Images Med 2025;11(2):1–4.ABSTRACT
Introduction: Acute pancreatitis is a rare complication of pregnancy; however, it can be associated with significant maternal and fetal mortality. Suggestive symptoms mimic multiple pregnancy and postpartum conditions, making the diagnosis difficult. This case report highlights diagnostic challenges and imaging findings in a patient with severe preeclampsia whose postpartum course was complicated by acute pancreatitis.
Case Report: A reproductive-aged patient presented, in the late second trimester, for preeclampsia with severe features by blood pressure and creatinine. Worsening of maternal kidney function and fetal status required urgent cesarean delivery. The postoperative course was complicated by severe abdominal pain. On initial imaging, there was postoperative fluid without any significant intra-abdominal pathology. However, worsening of the clinical condition and development of an acute abdomen required an exploratory laparotomy. Intraoperative findings were significant for intra-abdominal ascites and extensive saponification of the omentum, concerning for acute pancreatitis. Testing of the ascitic fluid revealed an elevated lipase level at 5,319 U/L, and a retrospective serum lipase level was 2,109 U/L. Despite a normal appearance of the pancreas on computed tomography (CT) scan of the abdomen, laboratory findings were confirmatory of the diagnosis of acute pancreatitis. The patient then underwent multiple abdominal explorations with direct peritoneal resuscitation. Recovery was progressive and discharge occurred three weeks postpartum.
Conclusion: Although rare, acute pancreatitis can complicate the postpartum course, especially in the setting of severe preeclampsia. This case underscores diagnostic challenges due to overlapping presentations. It is important to keep a high index of suspicion for acute pancreatitis in the differentials of postpartum abdominal pain, as late recognition and management are associated with significant morbidity.
Keywords: Cesarean, Pancreatitis, Postpartum, Preeclampsia
Introduction
Acute pancreatitis is a rare complication of pregnancy and, when it occurs, is associated with increased maternal and fetal mortality [1]. The presentation can be similar to multiple postpartum and postoperative complications, which can sometimes cause the diagnosis to be missed. We present a case of acute pancreatitis complicating the postpartum course of a 40-year-old patient with severe preeclampsia.
Case Report
A female patient presented in the late second trimester as a transfer from an outside hospital with new onset preeclampsia with severe features by blood pressure and worsening kidney function. The patient had multiple sustained severe range blood pressures requiring repeated intravenous antihypertensive medications. She was initiated on Nifedipine 30 mg extended release daily with good response. The patient had an elevated creatinine value at 1.63 mg/dL with a known baseline of 0.9. Given early gestational age, otherwise normal preeclampsia laboratory testing and the absence of other concerning symptoms of preeclampsia, she was expectantly managed through a steroid course and Magnesium infusion. However, subsequent deterioration in fetal status (category II fetal heart tracing non-responsive to resuscitative efforts) and worsening maternal renal function (creatinine at 1.70 mg/dL) led to the decision to proceed with urgent cesarean delivery performed under regional anesthesia. The procedure was uncomplicated and the abdomen was unremarkable. The patient delivered a male infant weighing 845 g with Apgar 6 and 9. The neonate was transferred to the neonatal intensive care unit in stable condition.
The patient had pain control issues starting postoperative day 2 despite a standard pain regimen. She complained of severe abdominal pain and extravasation of clear fluid was noted from the incision site. She had loss of appetite and given the concern for an ongoing intra-abdominal process, oral intake was held. Laboratory evaluation showed increasing white blood cell count at 30 × 106 and worsening kidney function with creatinine at 2.04 mg/dL, likely attributed to dehydration and non-steroidal anti-inflammatory drugs (NSAIDs) which were used against protocol. A renal ultrasound did not show any evidence of an obstructive process and urine microscopy showed findings consistent with both acute tubular necrosis and interstitial nephritis. She was hydrated and the NSAIDs were discontinued. Computed tomography (CT) scan of the abdomen and pelvis initially showed moderate diffuse ascites and a small amount of retroperitoneal free fluid; however, there was no concern for intra-abdominal infection or hemoperitoneum. A repeat CT was performed given worsening abdominal pain, and showed bilateral pleural effusions, body wall edema and no concern for bowel perforation. Serial physical exams then revealed an acute abdomen for which the patient then underwent an exploratory laparotomy on the fourth day postpartum.
Intraoperative findings were significant for extensive saponification of the omentum, mesentery, and peritoneum (Figure 1). General Surgery was consulted and noted thickening of the small bowel mesentery. The intraoperative findings were concerning for acute pancreatitis and early bowel ischemia. Therefore, the abdomen remained open for direct peritoneal resuscitation and re-exploration. A serum lipase obtained on the day of the exploratory laparotomy was only moderately elevated at 139 U/L. However, a retroactive serum lipase was obtained from postpartum day 2 and resulted at 2,109 U/L. Ascites fluid was collected from the surgery and analysis showed a lipase level at 5,319 U/L. All tissue and fluid cultures showed no microbial growth. The patient then continued to receive direct peritoneal resuscitation to reduce intraperitoneal edema and improve perfusion. She underwent multiple re-explorations, washouts and temporary closures. Her recovery course was complicated by abdominal wall wound necrosis, requiring multiple debridements and wound vacuum placement. The patient’s blood pressure and kidney function progressively normalized.
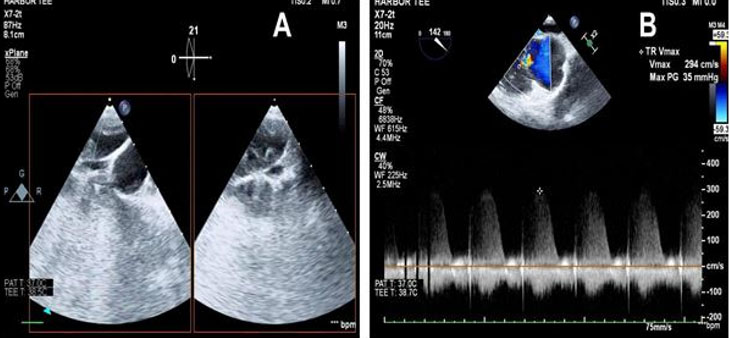
Given an elevated ascitic fluid and serum lipase with diffuse saponification seen intraoperatively, the patient was diagnosed with peritonitis caused by acute pancreatitis. The pancreas was unremarkable on both CT scans (Figure 2). Evaluation for a possible etiology of pancreatitis did not reveal a clear cause. Biliary imaging and autoimmune panels were negative. Triglycerides were normal. Calcium levels were mildly elevated. Of note, the patient’s mother had died from pancreatic cancer.
After stabilization, the patient was discharged on postpartum day 20 with scheduled outpatient follow-up visits with General Surgery and high-risk obstetrics team. Nifedipine was discontinued after normalization of blood pressures. The infant was discharged after 3 months in the neonatal intensive care unit.
Discussion
Acute pancreatitis is a rare complication in pregnancy with incidence varying between 1/12,000 and 1/1,000 [2]. Of these cases, 30% present in the postpartum period [3]. Biliary disease is the most common cause of acute pancreatitis in pregnancy and has been reported to be responsible for 67–100% of cases. This is due to hormonal changes altering bile flow and composition and generating a pro-lithogenic state. Other possible etiologies include alcohol use and hypertriglyceridemia, in part because estrogen alters lipid metabolism [4].
Preeclampsia is an obstetrical condition that increases the risk of maternal and fetal complications. Patients with a history of preeclampsia had a 1.68-fold increased risk of pancreatitis over those without preeclampsia [5]. Pancreatitis is strongly associated with preeclampsia (OR 4.21) and notably with preeclampsia with severe features (OR 7.85) [1]. Preeclampsia affects multiple organ systems and studies have shown increased risk of gallstones, diabetes, hypertension, hyperlipidemia, and hepatitis B and C infections which are also risk factors for pancreatitis. Microvascular abnormalities and visceral ischemia are other possible mechanisms through which preeclampsia increases the risk of pancreatitis in pregnancy [5].
Acute pancreatitis is diagnosed with the presence of two of the following three criteria: clinical presentation and symptoms, characteristic imaging findings and increased amylase or lipase to three times the upper limit of normal. Our patient had severe abdominal pain and anorexia in the immediate post-op period, elevated lipase that was not recognized until post-surgery and imaging findings that were not directly diagnostic. She also had findings consistent with bowel ischemia, elevated white blood cell (WBC), increased blood urea nitrogen (BUN), elevated lactate dehydrogenase (LDH), and creatinine which are concerning for severe pancreatitis [6].
Clinical manifestations typically include severe and constant epigastric pain, radiating to the back. However, presentation is not always typical and the onset of pain may be less abrupt, and poorly localized, as was the case with our patient which may have contributed to a delay in diagnosis. Other possible presentations include nausea and vomiting, abdominal distention, guarding, ileus, fever, respiratory symptoms including tachypnea, desaturation, cardiovascular symptoms including hypotension and tachycardia, and/or oliguria [4].
Possible imaging modalities include contrast-enhanced CT scan, magnetic resonance imaging (MRI), or transabdominal ultrasonography (US). Computed tomography findings consist of focal or diffuse enhancement of the pancreas, inflammatory fat stranding and/or peri-pancreatic fluid collection [4]. Despite the severity and acuity of presentation in this case, the pancreas was unremarkable on CT imaging twice. General abdominal and retroperitoneal fluid was noted and attributed to residual surgical irritant, preeclampsia or bladder rupture. However in retrospect, it could have been significant inflammatory fluid related to pancreatitis even with a normal-appearing pancreas. It is possible that MRI would have shown edema in the pancreas, which was not evident on CT where imaging findings often lag behind clinical presentation.
Comparing different studies showed that serum lipase offers a higher sensitivity than serum amylase in diagnosing acute pancreatitis [7] and also offers a larger diagnostic window, remaining elevated for a longer time. However, lipase may also be elevated as a result of other intra-abdominal pathologies arising from the stomach, bowel and hepatobiliary tract such as bowel obstruction and intestinal ischemia, the latter of which was an intraoperative finding in our patient’s case [8].
On reviewing our patient’s case, her clinical presentation is consistent with a rare case of acute pancreatitis in the setting of severe preeclampsia. This case highlights the importance of maintaining a high index of suspicion for pancreatitis in a patient with preeclampsia.
Conclusion
The differential diagnosis for abdominal pain in a patient with preeclampsia once obstetric causes have been ruled out is typically broadened to include less common but familiar etiologies like subcapsular hematoma, acute fatty liver of pregnancy and postoperative complications such as bleeding, bladder injury, bowel injury, etc. Acute pancreatitis is an easily diagnosed condition with possible serious sequelae if unmanaged that should be added to this list. Remembering this rare but possible complication in pregnant patients, especially with severe preeclampsia, leads to a higher index of suspicion which allows the provider to order appropriate tests and to consult appropriate teams. This approach can help with early diagnosis, management and monitoring for possible complications of acute pancreatitis.
REFERENCES
1.
Hacker FM, Whalen PS, Lee VR, Caughey AB. Maternal and fetal outcomes of pancreatitis in pregnancy. Am J Obstet Gynecol 2015;213(4):568.e1–5. [CrossRef]
[Pubmed]

2.
Zhang T, Wang G, Cao Z, Huang W, Xiao H, Wei H, et al. Acute pancreatitis in pregnancy: A 10-year, multi-center, retrospective study in Beijing. BMC Pregnancy Childbirth 2022;22(1):414. [CrossRef]
[Pubmed]

3.
Hofstrand R, Singhal M, Doad J, Watts R. Postpartum idiopathic pancreatitis complicated by acute necrotizing pancreatitis. Cureus 2023;15(1):e34002. [CrossRef]
[Pubmed]

4.
Szatmary P, Grammatikopoulos T, Cai W, Huang W, Mukherjee R, Halloran C, et al. Acute pancreatitis: Diagnosis and treatment. Drugs 2022;82(12):1251–76. [CrossRef]
[Pubmed]

5.
Huang JL, Chen WK, Lin CL, Kao CH, Shih HM. Preeclampsia and the risk of pancreatitis: A nationwide, population-based cohort study. Gastroenterol Res Pract 2020;2020:3261542. [CrossRef]
[Pubmed]

6.
Venkatesh NR, Vijayakumar C, Balasubramaniyan G, Chinnakkulam Kandhasamy S, Sundaramurthi S, Sreenath GS, et al. Comparison of different scoring systems in predicting the severity of acute pancreatitis: A prospective observational study. Cureus 2020;12(2):e6943. [CrossRef]
[Pubmed]

7.
Treacy J, Williams A, Bais R, Willson K, Worthley C, Reece J, et al. Evaluation of amylase and lipase in the diagnosis of acute pancreatitis. ANZ J Surg 2001;71(10):577–82. [CrossRef]
[Pubmed]

8.
Hameed AM, Lam VWT, Pleass HC. Significant elevations of serum lipase not caused by pancreatitis: A systematic review. HPB (Oxford) 2015;17(2):99–112. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
The authors acknowledge the use of open AI’s ChatGPT, version GPT-4, in some sections of the abstract. The technology was solely used to help with language refinement, grammar editing, and improving sentence structure of content written by the authors. The AI tool was not used to generate figures, tables, or novel data. All information and interpretations were generated by the research team and verified by the authors. The authors confirm that the content edited using AI tool was carefully reviewed and ensure accuracy and originality. The content is free from plagiarism.
Author ContributionsMarie Elise Abi Antoun - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Zeinab Kassem - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethelin Camille Cammock - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Charlotte McIntosh Lee - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sabrina Craigo - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Marie Elise Abi Antoun et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.